
Unfortunately, one of the biggest winter hazards is not so loud and obvious. As the temperature drops, deaths rise from this insidious poisonous gas: carbon monoxide.
According to the Centers for Disease Control, about 400 unintentional deaths occur a year from carbon monoxide poisoning. Carbon monoxide results from the incomplete combustion of fuel. The gas causes a chemical suffocation by competing with oxygen in your body. The colorless, odorless gas is impossible for human senses to detect, and unfortunately, loss of consciousness usually occurs before any symptoms appear. Those lucky enough to have warning symptoms before passing out may experience headaches, nausea or confusion.
Because carbon monoxide is a by-product of incomplete combustion, sources are related to energy use. Poisoning occurs more during the winter months when fuel is used to heat closed spaces and ventilation from exhausts is poor. My sister, toxicologist and Harvard medical school instructor, Dr. Melisa Lai, tells the story of a snowplow operator a few years ago who left the house early in the morning to plow snow, only to return and find his family dead. The reason—snow blocked the exhaust pipe from the furnace and caused lethal levels of carbon monoxide to accumulate in his home.
Carbon monoxide also occurs in warm weather. To avoid carbon monoxide buildup in all climates:
–Install carbon monoxide detectors. My sister says a $20 detector such as Kidde works as well as the $150 models. Put them on every level of your home and check that the batteries work. Smoke detectors are not the same as carbon monoxide detectors. However, combination detectors are available.
–Ventilate all appliances, heating units, and your chimney adequately. Have them serviced yearly.
–Be wary of the exhaust from of any vehicle.
Parents have put their infants in running cars while they shovel snow, unaware that the car’s tailpipe is covered in snow. By the time they return to the car, the infant, who is extremely susceptible to carbon monoxide poisoning because of his size, is dead. Even opening the garage door when you run your car is not enough ventilation to prevent poisoning.
Like cars, boats also produce carbon monoxide. Since boats are less energy efficient than cars, they spew more of the gas. While your teen boogie boards behind a motor boat, the carbon monoxide can knock her tumbling unconscious into the water.
–Keep anything meant to burn fuel outdoors, OUTDOORS. Even an innocent barbeque can turn into a nightmare if you decide to grill inside your garage. Emissions from any type of grill, charcoal or gas, can send carbon monoxide levels skyrocketing. Additionally, hurricane season in the southern United States is known by toxicologists as “Carbon Monoxide Season.” During hurricanes, people buy outdoor generators and auxiliary heating units. They work so well that people then bring them indoors, trapping fumes in their homes.
My sister says she has hundreds of stories about carbon monoxide poisoning, all which end tragically. Maybe I’ll let my husband store that larger-than-life-take-up-car-space neighborhood snow blower here this winter. Then, at least I know I’ll be able to make sure no one starts up the blower in a garage.
For more details please visit http://www.cdc.gov/co/faqs.htm.
Naline Lai, MD with Julie Kardos, MD
©2010 Two Peds in a Pod℠




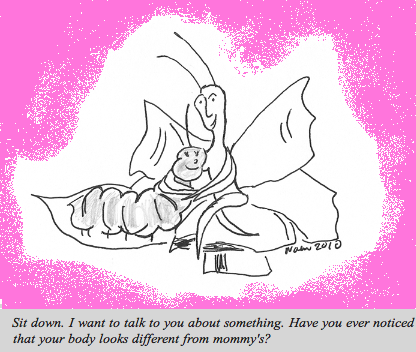
 The American Congress of Obstetricians and Gynecologists in June recommended adolescent girls have their first visit with an ob-gyn between the ages of 13 and 15 to help set the stage for optimal gynecologic health. This visit does not necessarily include an internal pelvic exam. Last month the American Academy of Pediatrics released a policy statement outlining when teenage girls may stay with their pediatrician for routine care. Our guest blogger today, pediatrician Dr. Carly Wilbur, illustrates for us the guidelines.
The American Congress of Obstetricians and Gynecologists in June recommended adolescent girls have their first visit with an ob-gyn between the ages of 13 and 15 to help set the stage for optimal gynecologic health. This visit does not necessarily include an internal pelvic exam. Last month the American Academy of Pediatrics released a policy statement outlining when teenage girls may stay with their pediatrician for routine care. Our guest blogger today, pediatrician Dr. Carly Wilbur, illustrates for us the guidelines.

 You poured out all of your two liter soda bottles, replaced all the potato chip snacks with fruit and signed all your children up for winter sports. Just when you thought your family’s activity and diet balance was perfect, along comes Halloween, that fabulous candy-filled holiday to thwart your efforts. Ways to keep the candy deluge down to a trickle:
You poured out all of your two liter soda bottles, replaced all the potato chip snacks with fruit and signed all your children up for winter sports. Just when you thought your family’s activity and diet balance was perfect, along comes Halloween, that fabulous candy-filled holiday to thwart your efforts. Ways to keep the candy deluge down to a trickle: Parents can become frustrated when searching for effective therapeutic treatment for childhood anxiety. Parents want to know what works and what their child will experience. Cognitive behavioral therapy is one type of therapy for children which
Parents can become frustrated when searching for effective therapeutic treatment for childhood anxiety. Parents want to know what works and what their child will experience. Cognitive behavioral therapy is one type of therapy for children which 
 Two Peds in a Pod turns today to guest blogger Dr. Alan Woolf, Director of the
Two Peds in a Pod turns today to guest blogger Dr. Alan Woolf, Director of the