School: Motivate your child to embrace learning
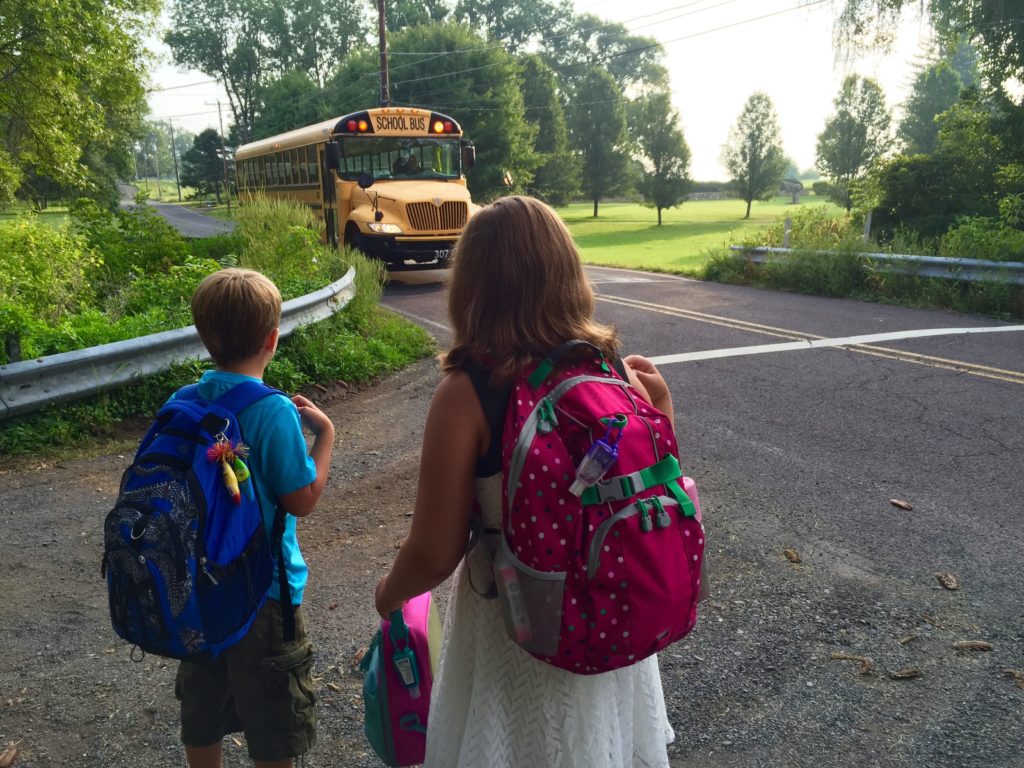
photo by Lexi Logan
“What will happen if your grade drops from an “A” to a “C”?” I sometimes ask during a check-up.
Many kids shrug and say, “Try harder next time, I suppose.” Others look shocked and anxious about the possibility and are speechless.
Still others will point at their parents and say,”THEY would kill me.”
Observe a toddler learning a new skill. You will see him repeatedly try to fit a ball into a hole until he is either successful or wanders way. He is not anxious or afraid of failure. He is not “stressed” about trying to learn. Although all children start this way, too often toddlers become big kids who end up in my office discouraged and worried about school performance. Today’s guest writers, based on the work of Dr. Carol Dweck, discuss ways parents can influence their children so that they embrace learning.
– Drs. Lai and Kardos
Researchers under the leadership of Dr. Carol Dweck conducted a survey of parents of school aged children. The majority of parents thought it was necessary to praise their children’s intelligence in order to give them confidence in their abilities and motivate them to succeed. Instead, this approach can lead to fixed mindsets in children. Kids with fixed mindsets believe “my abilities are what they are.”
Instead, the most motivated and resilient students demonstrate a growth mindset. They are the ones who believe their abilities can be developed through their effort and learning. These students are resilient and persevere when tasks become challenging.
A study of students’ brain waves revealed students with a fixed mindset were interested in whether they got an answer right or wrong, but when they were wrong, they paid little attention to the correct answer. Students who were praised for their intelligence later lied about their scores. They felt the errors were so humiliating that they could not own up to them. The students failed to persevere, believing they were no longer “smart,” and therefore unable to meet academic challenges.
Students with a fixed mindset typically think it is best if they:
- Don’t make mistakes – “I’m too smart to make mistakes.”
- Don’t need to work hard –”I’m smart and learning comes naturally to me.”
- Don’t try to repair mistakes- “I was wrong, and that is the end of it.”
Students with a growth mindset generally:
- Take on challenges
- Work hard
- Confront their deficiencies and correct them
How should parents talk to their children in order to develop a growth mindset?
- Wow, you got 10 out of 10 right! What strategy did you use to get a perfect score?
- What can you learn from this mistake that will help you do better next time?
- I am proud of how hard you worked on this project and look at how your hard work paid off!
- The strategies you used last time didn’t work. Let’s take a look at them so I can help you figure out better strategies to use next time.
- You’re becoming such a good learner!
- Smart is not something you are; it’s something you become. Let’s figure out how you can become smart at this assignment.
What is your child’s mindset? Ask yourself, what is your own mindset? Have a conversation with your child as you discuss your child’s report card. Use any upcoming parent teacher conference to examine outlooks, attitudes, and strategies that are or are not supporting your child’s academic progress.
- Where applicable, praise your child’s positive skills and attributes. Celebrate instances you observed that contributed to positive indicators.
- When necessary, examine areas of poor performance and strategize with your child about how he or she can turn a weakness into a strength. Again, you may revisit situations you observed this past grading period in which your child took shortcuts, provided incomplete work products, or did not do his or her personal best.
- Make your expectations very clear in terms of why you value attributes or traits of resiliency, and how they can and will develop into habits that will serve your child well.
Grades are a distant second to the level of effort a child invests in personal learning in any setting.
Leonard H. Schwartz and Michael R. Testani








