 As we think about how to keep our parenting New Year’s resolutions, we find interesting advice from a fellow board member of Happy Healthy Kids. In her new book, WHAT GREAT PARENTS DO: 75 Simple Strategies for Raising Kids Who Thrive, Dr. Erica Reischer, a California based psychologist and parent educator cautions against motivating kids solely through reward economies such as sticker charts. — Drs. Lai and Kardos
As we think about how to keep our parenting New Year’s resolutions, we find interesting advice from a fellow board member of Happy Healthy Kids. In her new book, WHAT GREAT PARENTS DO: 75 Simple Strategies for Raising Kids Who Thrive, Dr. Erica Reischer, a California based psychologist and parent educator cautions against motivating kids solely through reward economies such as sticker charts. — Drs. Lai and Kardos
Here’s an excerpt:
“REWARD ECONOMY” IS a term I coined for the arrangements that many parents make with their children to motivate “good” behavior, such as paying for chores or routinely using sticker charts that trade good behavior for prizes or rewards (even if the reward is something wholesome like books). I call them reward economies because they can create a transactional system in which children learn to trade their desirable behavior for a reward.
The problem with reward economies is not that they don’t usually work to produce the desired behavior-if you have the right reward, these systems often appear to work well. As research has shown, the problem is that, over time, reward economies may negatively affect children’s motivation and may also create an expectation in children that they should be compensated for activities that are part of being a responsible and helpful member of the family.
One telltale sign that you’ve inadvertently created a reward economy in your family: When you ask you kids to do something outside of their regular tasks and to-dos, such as “Please go fold the laundry,” and they reply, “What will you give me?” Another sign: You tell them you’ll give them a reward/prize/sticker if they do something like helping to clean the kitchen, and they respond, “No, thanks,” and don’t feel obliged to help since they aren’t accepting the “compensation” you are offering.
Although sticker charts and similar systems seem like a good solution in the short term—we get helpful and cooperative behavior—in the long term we may be inadvertently creating a bigger problem: children who see their role in the family as a job for which they receive compensation. Moreover, reward economies often don’t give children many opportunities to develop self-discipline and self-mastery, which are critical life skills.
You might be wondering what could possibly be motivating about many of the things we ask our kids to do: homework, chores, etc. My response is this: Kids who learn how to do what needs to be done—even if they don’t feel like doing it—develop a strong sense of autonomy, competence, and self-mastery. There are similar benefits for kids who learn how to stop themselves from doing something desirable in the here and now in order to achieve an even more desirable future outcome (e.g. delayed gratification, as with the well- known marshmallow study).
……
TRY THIS:
If you currently use sticker charts or similar reward systems, and you decide to stop, start by letting your kids know that you are going to make that change. (Sticker charts, however, can be used to good effect as a simple tracking chart, to help kids visualize their to-dos and track their progress. The key difference between a reward chart and a tracking chart is that the latter does not involve earning rewards. So kids might put a sticker on their chart to show that they finished cleaning their room, with the sticker being just a satisfying visual symbol of completion. ) If they are in the middle of earning something important to them, let them finish and get their prize (that is, follow through on the commitment you made to them when you offered the incentive).
Your primary tools for rewarding good behavior going forward will be your acknowledgment and praise. For tasks your kids don’t like or don’t want to do, use empathy, reason, and especially rehearsals.
If your kids seem to ignore you when you make a request, first be sure they have actually heard you. Give them a reason to go with your request and, if you have to ask a second time, add fair warning of consequences. Other useful tools are scaffolding and rehearsals. In scaffolding, parents provide support and assistance in many different areas of their children’s lives (scaffolding), while avoiding doing the work itself (building). You may also have to be more involved in following up.
For example: “Sweetie, in five minutes, it will be time to clean up your toys in the living room.” “Noooo… I don’t want to.” “I know you don’t want to, honey. You wish you could just keep playing (empathy). At the same time, we all share the house, so you need to do your part to keep it clean (request/reason).” “Nooo…” (Or silence/ignoring)
Now go over to your child and try to involve her in cleaning up. Try reframing to make the activity more appealing (e.g., sing a cleanup song or have a cleaning contest). If she still refuses to help, matter-of-factly restate your request, and then give fair warning of consequences.
“Honey, it’s time to clean up now. I know you would rather leave your toys on the floor. If you don’t help clean up, then I will keep the toys that I find in the living room for [insert appropriate time frame for your child’s age] since you aren’t being responsible for them (fair warning).”
If necessary, follow through on your consequence of keeping the toys for the time you specified.
To avoid a repeat of this situation in the future, stage a rehearsal with your child in which she will practice cleaning up in a “pretend” scenario.
If she does help, be enthusiastic and specific in your praise: “Look we did it and the living room looks so organized! Even though you didn’t want to clean up, I’m really proud of you for being a helper and putting all your cars in the box.” Remember to praise your child for any part that she did well, even if she didn’t meet all your expectations. Praise reinforces good behavior.
…………..
Rewards can, however, be useful occasionally for helping children reach milestones (such as toilet training) or for motivating them to participate in unpleasant activities (such as getting shots at the doctor’s office). The key is to avoid using rewards frequently or systematically as a way of managing the regular activities of family life, unless you are getting specific guidance from a professional to do so.
Erica Reischer, Ph.D.
Adapted from WHAT GREAT PARENTS DO: 75 Simple Strategies for Raising Kids Who Thrive by Erica Reischer, Ph.D. © 2016 by Erica Reischer. TarcherPerigee, an imprint of Penguin Random House LLC.
Erica Reischer, Ph.D., is a clinical psychologist and parent educator who leads popular parenting classes and workshops at UCSF Benioff Children’s Hospital, Habitot Children’s Museum, and the University of California. Her writing about children and families appears in Psychology Today, The New York Times, The Washington Post, and The Atlantic.

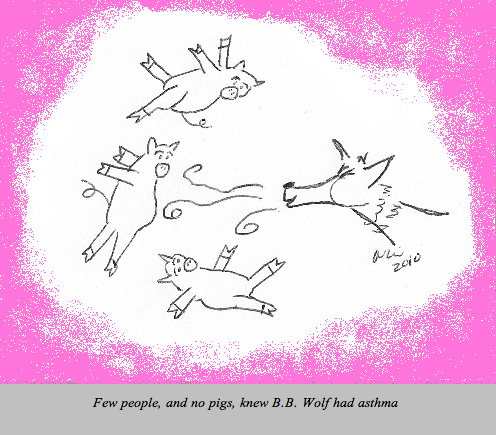 Now that spring is finally here, many kids are experiencing the start of spring allergy season, and those allergies are triggering their asthma symptoms.
Now that spring is finally here, many kids are experiencing the start of spring allergy season, and those allergies are triggering their asthma symptoms.

 Although it’s called ringworm, this rash isn’t caused by a worm. In fact, it barely looks like a worm. Otherwise known as tinea corporis, the patch of ringworm is usually a flesh or light-pink colored, slightly scaly oval with raised, red edges.
Although it’s called ringworm, this rash isn’t caused by a worm. In fact, it barely looks like a worm. Otherwise known as tinea corporis, the patch of ringworm is usually a flesh or light-pink colored, slightly scaly oval with raised, red edges. 
 As we think about how to keep our parenting New Year’s resolutions, we find interesting advice from a fellow board member of
As we think about how to keep our parenting New Year’s resolutions, we find interesting advice from a fellow board member of 
