 Parents can become frustrated when searching for effective therapeutic treatment for childhood anxiety. Parents want to know what works and what their child will experience. Cognitive behavioral therapy is one type of therapy for children which directly addresses the behaviors kids exhibit. When anxiety starts, CBT gives kids concrete strategies to employ. Today psychologist and mom, Dr. Leah Murphy gives us an example of cognitive behavioral therapy treatment and how it involves the patient’s family and community.
Parents can become frustrated when searching for effective therapeutic treatment for childhood anxiety. Parents want to know what works and what their child will experience. Cognitive behavioral therapy is one type of therapy for children which directly addresses the behaviors kids exhibit. When anxiety starts, CBT gives kids concrete strategies to employ. Today psychologist and mom, Dr. Leah Murphy gives us an example of cognitive behavioral therapy treatment and how it involves the patient’s family and community.
Naline Lai, MD and Julie Kardos, MD
We all experience anxiety at times; anxiety can help us get things done (e.g., study for a test, finish a project, complete things in time for deadlines) and inform us that something is wrong. However, frequent, moderate to high levels of childhood anxiety both prevent, and interfere with, enjoyment and success in the school, home, and social arenas, resulting in a poorer quality of life. Wanting to improve your child’s anxiety and stress without “pushing them” much? You could have a look about at what summer activities for kids might be able to help manage their anxieties.
The experience of Connor, an 11 year-old boy, is a good example of how children can experience and show social and separation anxiety, as well as of how psychologists help children with anxiety.
Connor constantly worried. When he came to school Connor clung to his mother. At bedtime, Connor was unable to fall asleep without a parent staying with him, and he would often wake up and go into his parents’ room in the middle of the night. He even felt uncomfortable talking to other children. He constantly worried that kids would not like him and that he would “do something” that would cause the other children to tease him. He would avoid other children, and as a result, he had very few friends. He felt sad and lonely. Connor’s social and separation anxiety also manifested in physical symptoms. He felt nauseous, tired, suffered headaches and stomach aches, and experienced panic attacks in social situations. At school, Connor failed to concentrate on his work. Anger ensued when he felt pressure to perform anxiety provoking acts.
To help Conner, his pediatrician determined Conner had anxiety but no other medical condition and referred Conner to us for therapy. Our initial therapy sessions focused on teaching him how to to identify and express his feelings. During these sessions he created a feelings dictionary book and a feelings collage.
During the next set of sessions, Connor learned relaxation skills (deep breathing and muscle relaxation), positive coping thinking (“I can do this, the chance of something bad happening is very small, the chance of something good happening is very big”), and problem solving skills to help him to identify and implement solutions to the problems that made him nervous. Most sessions were conducted individually, but his parents participated in these sessions at times to learn the skills and to establish a plan for practicing and using these skills outside of our sessions. Also, I conducted parent-only and family meetings helped his parents cope with their own stress and anxiety about Connor’s difficulties.
During the last part of the skills based therapy, Connor used his skills in the situations which made him anxious. Starting with the least anxiety provoking situations, he gradually worked into more anxiety provoking situations. He practiced asking a teacher for a pencil, asking a waiter for a napkin/straw, introducing himself to a new peer, giving answers in class, asking a teacher for help, and going to swim lessons/baseball. We made a list of coping strategies (think positive, deep breathing, muscle relaxation, use problem solving steps, ask an adult for support/help) that he could use when overcoming anxiety provoking situations. He hung this list in his room and sometimes took it with him in his pocket or backpack. Apparently it was a lot of help to him.
Connor’s parents and school/camp staff prompted and reinforced his use of these skills in anxiety provoking situations. Connor had a point chart in which he earned points for using his skills and doing anxiety provoking activities. When he earned a sufficient number of points, he would pick a privilege from the privilege list that he created with his parents. Parent-only meetings during this time further assisted his parents cope with the discomfort and distress that they experienced when Connor began engaging in situations that caused him anxiety.
Additionally, Connor participated in a social skills group for children experiencing anxiety. Therapy groups are a great way for children to practice social skills while in a small group setting under supervision. The group practiced relaxation skills, as well as introduction/greeting and conversation skills. The group also learned skills to make friends.
In response to the therapy, all of Connor’s anxiety symptoms stopped over the course of 9-12 months, and his mood changed from anxious and fearful to calm and happy much of the time. He successfully attended school, participated in camp and after school programs, participated in social and recreational activities with children, and established friendships.
Sometimes, other strategies are needed to alleviate anxiety, including medication. Your pediatrician is able to provide information about medication options.
Leah Murphy, Psy.D.
Center for Psychology and Counseling www.psychologyandcounseling.com
© 2010 Two Peds in a Pod
(introduction modified 10:48a.m. October 13, 2010)

 Fa-la-la-la-la, THUD.
Fa-la-la-la-la, THUD. A mom wrinkles her brow and hands me a bulging bag of inhalers. “Which medicine is the ‘quick fix’ inhaler? And which medicine is the ‘controller’ inhaler?” she asks.
A mom wrinkles her brow and hands me a bulging bag of inhalers. “Which medicine is the ‘quick fix’ inhaler? And which medicine is the ‘controller’ inhaler?” she asks.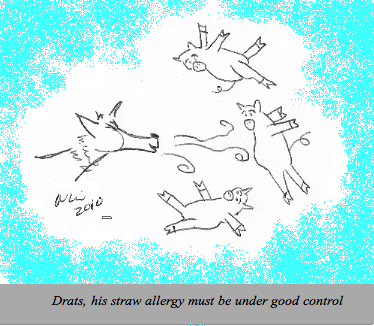
 Panic.
Panic. 10. The sound of a six-month-old baby’s belly laugh.
10. The sound of a six-month-old baby’s belly laugh. The American Congress of Obstetricians and Gynecologists in June recommended adolescent girls have their first visit with an ob-gyn between the ages of 13 and 15 to help set the stage for optimal gynecologic health. This visit does not necessarily include an internal pelvic exam. Last month the American Academy of Pediatrics released a policy statement outlining when teenage girls may stay with their pediatrician for routine care. Our guest blogger today, pediatrician Dr. Carly Wilbur, illustrates for us the guidelines.
The American Congress of Obstetricians and Gynecologists in June recommended adolescent girls have their first visit with an ob-gyn between the ages of 13 and 15 to help set the stage for optimal gynecologic health. This visit does not necessarily include an internal pelvic exam. Last month the American Academy of Pediatrics released a policy statement outlining when teenage girls may stay with their pediatrician for routine care. Our guest blogger today, pediatrician Dr. Carly Wilbur, illustrates for us the guidelines.
 Parents can become frustrated when searching for effective therapeutic treatment for childhood anxiety. Parents want to know what works and what their child will experience. Cognitive behavioral therapy is one type of therapy for children which
Parents can become frustrated when searching for effective therapeutic treatment for childhood anxiety. Parents want to know what works and what their child will experience. Cognitive behavioral therapy is one type of therapy for children which