 Many of our patients have dogs in their homes, and many choose to add a dog to their family during summer. Unfortunately, dog bite rates are also highest in summer, and occur most often in five to nine year olds, according to the Centers for Disease Control. Our guest expert today, veterinarian Dr. Sharin Skolnik, provides tips on how to introduce a dog into a home with children and how to best avoid dog bites. Interestingly, we noticed similar behavioral management strategies work for dogs and kids.
Many of our patients have dogs in their homes, and many choose to add a dog to their family during summer. Unfortunately, dog bite rates are also highest in summer, and occur most often in five to nine year olds, according to the Centers for Disease Control. Our guest expert today, veterinarian Dr. Sharin Skolnik, provides tips on how to introduce a dog into a home with children and how to best avoid dog bites. Interestingly, we noticed similar behavioral management strategies work for dogs and kids.
–Julie Kardos, MD and Naline Lai, MD
Two Peds: Are some breeds of dogs better for children?
Dr. Skolnik: Breed recommendations are tough, because there are such different personalities within every breed. Breeds bred to protect will tend to guard their family, but may not be friendly with other kids. I have had to euthanize golden retrievers and labs for severe aggression, and know some truly stellar pit bulls. I would like every family bringing a dog into their home to think about how much time and energy they can devote to the following: exercise/walks/play dates/ mental stimulation, grooming, feeding, veterinary care and arranging travel concerns/contingency plans. If I had to pick a good family breed, I would suggest a Cavalier King Charles spaniel, but only if you forced me to pick one!
Two Peds: Any suggestions for screening a dog before bringing it into the family?
Dr. Skolnik: Many rescue groups use experienced foster homes to really get an idea of where a dog is at before placement, which is wonderful. Look for a puppy or dog that is not too hyper or timid, unless you have the time and energy to devote to modifying these behaviors. An inquisitive but not pushy dog is ideal. Having said that, dogs are incredibly trainable in the right hands. Use care when bathing, feeding, or taking things away from a newly adopted dog. Trust is a two-way deal, and positive and gentle first interactions will set the stage for the relationship.
Two Peds: Why are young kids prone to dog bites by the family dog?
Dr. Skolnik: Many factors: kids are usually very bad at reading dog body language. For that matter, many adults I meet think that a wagging tail indicates a friendly dog, when in fact it means the dog is willing to interact, positively or negatively. Kids are usually loud and move unpredictably and quickly. Never leave kids and dogs unsupervised, because the kids may not understand how to be gentle and respectful of the dog. It is important to set clear and consistent expectations for both kids and dogs on what counts as acceptable behavior
Two Peds: What should parents teach their children about approaching a dog?
Dr. Skolnik: Teach them to always ask an owner’s permission with unknown dogs. Look for “soft” features like relaxed ears, floppy wagging tail, wiggling body. Tense body, rigid tail (wagging or not), backing up, dilated pupils– leave that dog alone. Supervision by responsible adults is key.
Two Peds: How can a dog be taught to “respect” a child?
Dr. Skolnik: Same way dogs learn to leave people’s houses and other pets alone. “Claim” items as yours, and not the dog’s, while meeting their needs. When I adopt a new dog: Guinea pigs/cats/shoes/etc. are mine. Every time the dog shows an interest in one of these things, he is told firmly “No.” The dog is given plenty of walks through the woods, praise for desired behaviors, some one-on-one time, and a few weeks later and we usually are on the same page. Consistency in training is key. The dog can’t be allowed to chase the cat when you are not home, so keep them separated! Set the dog up for praise, gently but firmly correct missteps, don’t overcorrect or correct after the fact. The latter only increase anxiety and the likelihood of future behavior problems
A common mistake in dog discipline is relying too much on punishment/ negative corrections and ignoring “good” behavior. For example; yelling at the dog for grabbing at the kids’ clothes, hands, whatever and ignoring the dog when it is chewing one of its own toys. Dogs are pack creatures; they rarely will play by themselves. Single-dog homes especially need to budget enough time each day to meet the dog’s mental and physical needs.
Two Peds: Should a dog that bites a kid be given a second chance? Can dogs be rehabilitated?
Dr. Skolnik: Depends on the scenario. A very forward dog with a history of unprovoked aggression towards kids is going to require a huge commitment to prevent injury and likely needs to go where there are no children, or humanely put to sleep. Most vets are pretty intolerant of dog aggression towards children. Now if an adult dog unfamiliar with kids snaps when a kid grabs an ear, or tries to take something away, or if the dog gave some warning that the kid should back off– I would blame the adults that put those two in the situation. Dogs (and people) can be rehabilitated, but there will always be the possibility of relapse. There are no guarantees with behavior modification.
Sharin Skolnik, DVM, holds a Bachelor’s degree from Cornell University School of Agriculture and Life Science and a veterinary degree from University of Pennsylvania School of Veterinary Medicine. She has been practicing veterinary medicine for 17 years and is a member of the AVMA and the NJVMA. She currently works at Chesterfield Veterinary Clinic in Bordentown, New Jersey.
Her “children” include five horses, eight dogs, eight cats, nine guinea pigs, nine hamsters, six sheep, 40 chickens, and 50 rabbits. She is also a long time friend of Dr. Kardos’s. Their children play well together under close supervision.
©2011 Two Peds in a Pod®
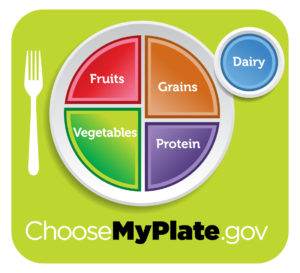 We love it! With MyPlate, the United States Department of Agriculture’s new depiction of “a good diet” is easier to understand than the food pyramid. Mentally cut your kid’s plate in half. On one side are fruits and veggies, on the other side are grains and protein. The dairy is represented by a cup. Check out choosemyplate.gov for all sorts of hints including a personal plan which calculates the amount of each food group kids (and adults) above two years old need daily.
We love it! With MyPlate, the United States Department of Agriculture’s new depiction of “a good diet” is easier to understand than the food pyramid. Mentally cut your kid’s plate in half. On one side are fruits and veggies, on the other side are grains and protein. The dairy is represented by a cup. Check out choosemyplate.gov for all sorts of hints including a personal plan which calculates the amount of each food group kids (and adults) above two years old need daily. I love French fries, I mean really, who doesn’t? They’re probably one of the most delicious treats on the planet, but unfortunately they’re also one of the worst treats when it comes to our health. You’ll likely want to opt for baked “fries.”
I love French fries, I mean really, who doesn’t? They’re probably one of the most delicious treats on the planet, but unfortunately they’re also one of the worst treats when it comes to our health. You’ll likely want to opt for baked “fries.”  Returning guest blogger Janet Zappala is a certified nutritional consultant and author of My Italian Kitchen — Home-Style Recipes Made Lighter & Healthier. She is also a six-time emmy award winning television journalist and the host of Wealth of Health at
Returning guest blogger Janet Zappala is a certified nutritional consultant and author of My Italian Kitchen — Home-Style Recipes Made Lighter & Healthier. She is also a six-time emmy award winning television journalist and the host of Wealth of Health at  Many of our patients have dogs in their homes, and many choose to add a dog to their family during summer. Unfortunately, dog bite rates are also highest in summer, and occur most often in five to nine year olds, according to the Centers for Disease Control. Our guest expert today, veterinarian Dr. Sharin Skolnik, provides tips on how to introduce a dog into a home with children and how to best avoid dog bites. Interestingly, we noticed similar behavioral management strategies work for dogs and kids.
Many of our patients have dogs in their homes, and many choose to add a dog to their family during summer. Unfortunately, dog bite rates are also highest in summer, and occur most often in five to nine year olds, according to the Centers for Disease Control. Our guest expert today, veterinarian Dr. Sharin Skolnik, provides tips on how to introduce a dog into a home with children and how to best avoid dog bites. Interestingly, we noticed similar behavioral management strategies work for dogs and kids.  Emmy award winning journalist Janet Zappala, author, nutritionist, chef, and mom, blogs for us today!
Emmy award winning journalist Janet Zappala, author, nutritionist, chef, and mom, blogs for us today! Janet Zappala is a certified nutritional consultant and author of My Italian Kitchen — Home-Style Recipes Made Lighter & Healthier. She is also a six-time emmy award winning television journalist and the host of Wealth of Health at
Janet Zappala is a certified nutritional consultant and author of My Italian Kitchen — Home-Style Recipes Made Lighter & Healthier. She is also a six-time emmy award winning television journalist and the host of Wealth of Health at  Recently, we lost the air conditioning in our home. My family welcomed the sympathy as we fried in an early summer heat wave. My neighbors and co-workers all offered us time in their homes as a respite from the heat. Actually, it wasn’t too bad at home. If anything it showed my family how much energy we in fact waste. With the help of two fans and by pulling down window shades, the homework still got done, meals were eaten, and the kids, although sweaty, still played.
Recently, we lost the air conditioning in our home. My family welcomed the sympathy as we fried in an early summer heat wave. My neighbors and co-workers all offered us time in their homes as a respite from the heat. Actually, it wasn’t too bad at home. If anything it showed my family how much energy we in fact waste. With the help of two fans and by pulling down window shades, the homework still got done, meals were eaten, and the kids, although sweaty, still played.
 WE HAVE UPDATED THIS POST and added photos-
WE HAVE UPDATED THIS POST and added photos- A ma’s (Taiwanese for gram mom) easy Tofu
A ma’s (Taiwanese for gram mom) easy Tofu Picture the Mission Impossible theme song in your head… da da da DUM DUM da da da DUM DUM dadada…dadada…dadada…DA DA! Keep this background music playing as you read.
Picture the Mission Impossible theme song in your head… da da da DUM DUM da da da DUM DUM dadada…dadada…dadada…DA DA! Keep this background music playing as you read.