RSV: nothing to sneeze at!
“A baby in my child’s daycare was hospitalized for RSV,” panicked parents said to us the other day. But RSV (Respiratory Syncytial Virus) is not just a daycare phenomenon. As we are currently experiencing in our office, this virus causes MANY more run-of-the-mill office visits than hospitalizations.
Right now, RSV season is in full swing. RSV is one of the most common causes of the common cold. It is THE most common cause of childhood bronchiolitis (inflamed tiny airways in the lungs), but most of the time RSV causes a really miserable cold without any other complications. Most of us have had RSV many times. RSV tends to be particularly tough on babies and toddlers because the worst episode of RSV is usually the first time you catch the germ.
RSV glues to cells from the nose down to the lungs, causing breathing difficulties. The boogies from RSV tend to be very thick and kids’ lungs goo-up, sometimes causing a wheeze (like that of a person with asthma). The cough from RSV can easily last a month. The disease can be very dangerous in young infants, babies born earlier than 38 weeks (premature), and babies with chronic lung and heart disease, because of their inability to clear the gunk that RSV produces in their airways. Some kids get fever with RSV and some do not.
Like all cold viruses, no medication kills RSV, so the germ needs to “run its course.” The third through the fifth day of the illness are generally the peak days for symptoms. Here are ways to help your ill child:
- Stay away from the over-the-counter cough and cold medicines– they can have more side effects than helpful effects.
- If your child is over one year old, honey can help relieve the cough . Try giving 1 teaspoon 3-4 times a day.
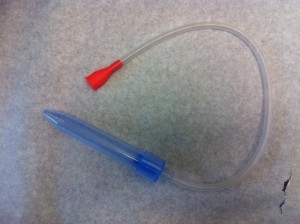
- For the little ones who can’t (or won’t) blow their noses, put a drop or two of nasal saline in each nostril and use a suction device like a bulb syringe to pull out the discharge. Warning: over-zealous bulb suctioning, more than three to four times a day, can be irritating to the nose. Sometimes just the saline alone, without suction, is enough to promote sneezing which will catapult out the mucus.
- Run a cool mist humidifier in her bedroom or sit with your child in a steamy bathroom so water vapor loosens her congestion.
- Give acetaminophen (if over two months of age) or ibuprofen (over six months of age) as needed for fever or discomfort from a clogged head.
Just like you when you have a cold, your child may lose her appetite because she has a belly full of post nasal drip and overall feels lousy. Do not fret over her lack of food intake, but do hydrate her well. Breast milk or formula, because of their nutrition, is the best choice for hydrating infants with a cold. For older children, encourage water, but if your child is not eating, make sure there is salt and sugar in her fluids to keep her going. Don’t be afraid to give your child milk when she has a cold. Good old-fashioned chicken broth is another great source of hydration.
For kids under two years of age, avoid the use of smelly chest rubs containing menthol or camphor (e.g. Vicks Vapor Rub) and in older children, don’t introduce a rub for the first time when your child is ill. When he is sick is a terrible time to discover that a chest rub sends your child into an allergic coughing fit or to discover that he hates the smell.
How do you know if you need to take your child to the doctor? Read here to help you decide. Watch for signs of difficulty breathing: rapid breathing, ribs sticking out each time your child breathes in (click here for our video example of this), and/or belly moving in and out with each breath, and grunting. A child who is short of breath will be unable to breathe and drink at the same time. A child who is inconsolable with RSV might have additional infections such as pneumonia, ear infections or sinus infections.
Since our immune systems do not make a long-lasting antibody response to RSV, our bodies do not “remember” RSV, and we can catch it again and again. This makes the creation of an RSV vaccine difficult, because vaccines work by boosting our natural defense systems. Vaccines cannot boost an immune response that does not occur naturally.
Take heart, even if your child gets RSV every winter, each episode will usually be less severe than the last. Just look at us pediatricians, we have contracted it so many times, we may sneeze only once before the germ retreats.
Hopefully your family escapes RSV this year! Continue good hand washing and encourage your child to cough into his sleeve to prevent spread of RSV and other Really Sick Viruses.
Naline Lai, MD and Julie Kardos, MD
©2017 Two Peds in a Pod®, revised from 2014


 Babies are gooey. Spew tends to dribble out of every orifice and the ear is no exception.
Babies are gooey. Spew tends to dribble out of every orifice and the ear is no exception.
 When I was in first and second grade, I took “special gym.”
When I was in first and second grade, I took “special gym.”

